Arthritis / Degenerative Joint Disease (DJD)
What does “Wear & Tear” really mean?
ARTHRITIS / DEGENERATIVE JOINT DISEASE (DJD)
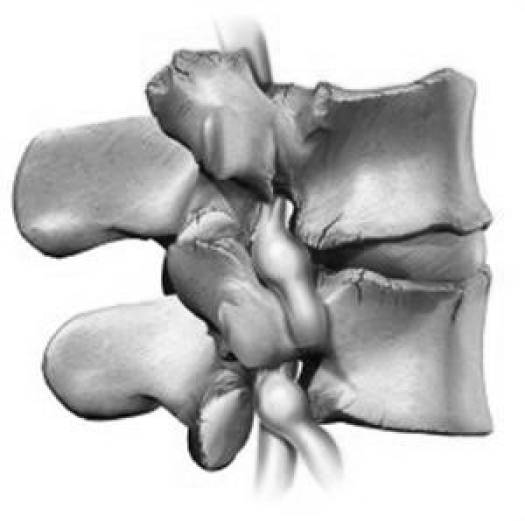
Arthritis,Wear ‘n Tear, Joint Degeneration, Spondylosis are conditions where the joints gradually deteriorate over time. In the lumbar spine degenerative joint disease has several other names such as lumbar spondylosis, arthritis or more commonly just simple wear ‘n tear. As with all conditions there is a scale of severity and the degree of symptoms is usually related to the extent of change. Each lumbar segment consists of three separate joints all of which function as a combined unit. The main joint is located in the front of the spinal column and is formed by the intervertebral disc and the surface of each vertebra. The other two joints are known as the facet joints (zygapophyseal joints) and are located on each side of the spinal column.
THE INTERVERTEBRAL JOINT
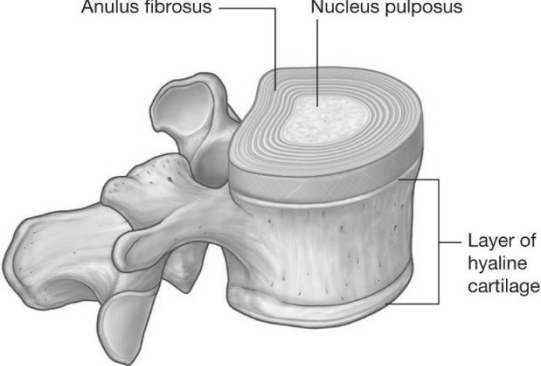
The intervertebral joint of the lumbar spine is a unique type of joint whose architecture is specific to handling compression.
In most joints the bone surfaces are covered with articular cartilage which forms a smooth friction free surface allowing easy movement. In the case of the intervertebral joint the disc effectively becomes the joint surface between two adjacent vertebrae.
In the lumbar spine the main function of the intervertebral disc is to act as a shock absorber to control compressive loads on the spine. The disc also allows some stretching and twisting depending on the direction of movement and there is a very small amount of sliding motion at the disc with these normal movements.
Disc Mechanics
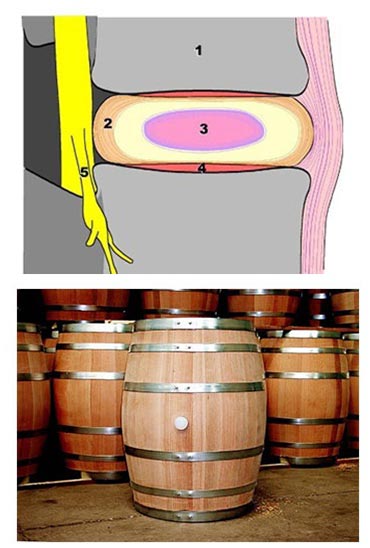
When the intervertebral disc is subjected to compressive load the central portion (nucleus pulposus) tries to expand sideways but is restrained by the rings of the annulus fibrosis. The annulus is an elastic structure but more rigid than the nucleus and it resists the pressure to deform – much like the metal rings on a barrel.
In the lumbar spine each disc is about 1½ cm thick when healthy. A healthy disc is defined as one where the outer casing (annulus) is fully intact with all of the rings continuous and no breaks visible. The central portion of the disc (nucleus) should contain its normal amounts of water in order to be able to function effectively as a gel shock absorber.
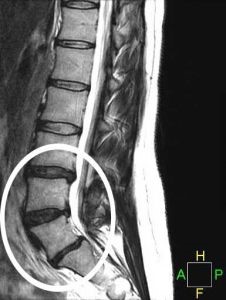
MRI Scans allow us to measure the height of the intervertebral disc, to visualise if there is any bulging, to determine if any bulging visible is contained by the outer annulus or whether it has in fact protruded breaking the outer casing of the annulus.
The normal MRI scan (shown below) is a side view with the abdomen on the left and the back on the right. This square (grey) blocks are cross-sections through each bony vertebra and the intervertebral disc is the black structure in between. Note
- the height of each disc is very similar
- there are no obvious bulges (discs tends to bulge backwards)
- there are clearly defined white, oval structures within the middle of the disc. These represent healthy nucleus pulposus which are properly contained within the disc and retaining normal water content allowing it to function like a spongy gel.

When degenerative changes occur in the intervertebral joint the MRI scan shows a number of changes (as indicated below). The disc space height reduces, the surfaces of the vertebrae can become buckled and distorted, the central of portion of the disc disintegrates losing water content and often becoming invisible.
This has very direct effects on the ability of the spine to absorb shock and impact. This can also be associated with some bulging of the disc which is shown towards the top of the circle in this MRI.
Because each part of the vertebrae is connected when these types of the changes occur to the disc and intervertebral joint it has direct effects on the two facet joints behind the disc on either side. In the lumbar spine, normally the facet joints act like guide rails to control the direction of movement and are not significant weight-bearing joints (best estimates suggest that about 20% of bodyweight goes through the facet joints). Unfortunately when the disc height reduces and the function of the disc as a shock absorber diminishes this ends up transferring pressure to the facet joints and over time can result in degenerative change.

In its simplest form these changes may just be joint surface, capsular irritation or sensitivity of the small sensory nerves in the area.
However, this can progress to: 1. Wearing away of the joint surfaces.
2. Thickening around the margins of the facet joints making them stiff to move and blocking movement in certain directions.
There is another complication apart from restricting movement which is:
3. The possibility of nerve irritation/compression. The space where the nerve emerges from each joint (known as the intervertebral foramen), is really a bony tunnel formed by the disc and vertebra in front and the facet joints behind. When the disc height reduces, the back sections of the vertebra and disc push backwards towards the nerve root while at the same time thickening around the facet joints behind start to narrow the space from the other side. This is sometimes referred to as foraminal encroachment.
Symptoms
Because of the widespread changes which occur in degenerative joint disease in the lumbar spine the symptoms are related to which structure is most sensitive. It is generally a condition which affects people over 50. If the nerve is being compressed the predominant symptoms are in the leg. Frequently this can be related to position – either lying or standing / walking for any period of time. Frequently, in these type of cases there isn’t much back pain which can be deceptive in identifying the underlying cause of symptoms.
When the nerve isn’t involved and symptoms originate from the facet joints this is usually specific pain on either side of the spine and patient often want to press / rub the area. Symptoms can be on one side or both (bilateral). Typically twisting, extending backwards and impact/jarring aggravate symptoms.
In many cases there is no specific type of pain just a general stiffness and discomfort across the lower spine in which case it is not possible to identify the specific/structure causing pain other than to say that pain is associated with generalised degenerative joint disease (DJD).

Treatment
Physiotherapy treatment of degenerative joint disease (DJD) really depends on the stage and severity of the condition. It is important to note that although the MRI scans may show significant change it does not mean that symptoms cannot be improved.
Usually a trial course of 3-4 sessions of manual therapy can determine if the condition is likely to respond, the rate of progress to be expected, the degree of potential and the prognosis. Obviously is not possible to fully reverse degenerative change but it is possible to improve the quality of movement and pain level.
This is achieved with specific joint mobilisation, improved postural alignment (if a contributory factor), identification and addressing flexibility deficits around the hips / spine contributing to increased pressure and ensuring that the muscle control is optimal to redistribute pressure from the sensitised joints.
BACK PAIN – SPECIFIC CONDITIONS
JOIN OUR MAILING LIST
EMAIL: